This illness, along with its various forms, is particularly destructive as individuals transition from normal functioning to experiencing difficulties with memory and cognitive abilities within a few years. Moreover, the disease is ultimately fatal.
The recent findings, published in the journal Alzheimer’s & Dementia, suggest that understanding the connection between gut infections and Alzheimer’s could contribute to effective treatment and prevention strategies.
Most humans are thought to encounter this virus, known as cytomegalovirus or HCMV, in the early decades of life. Cytomegalovirus is one of nine herpes viruses, distinct from those transmitted sexually.
In certain individuals, this virus may result in a persistent gut infection, residing in the gastrointestinal tract.
Eventually, the virus might reach the brain through the vagus nerve, a vital pathway linking the gut and brain.
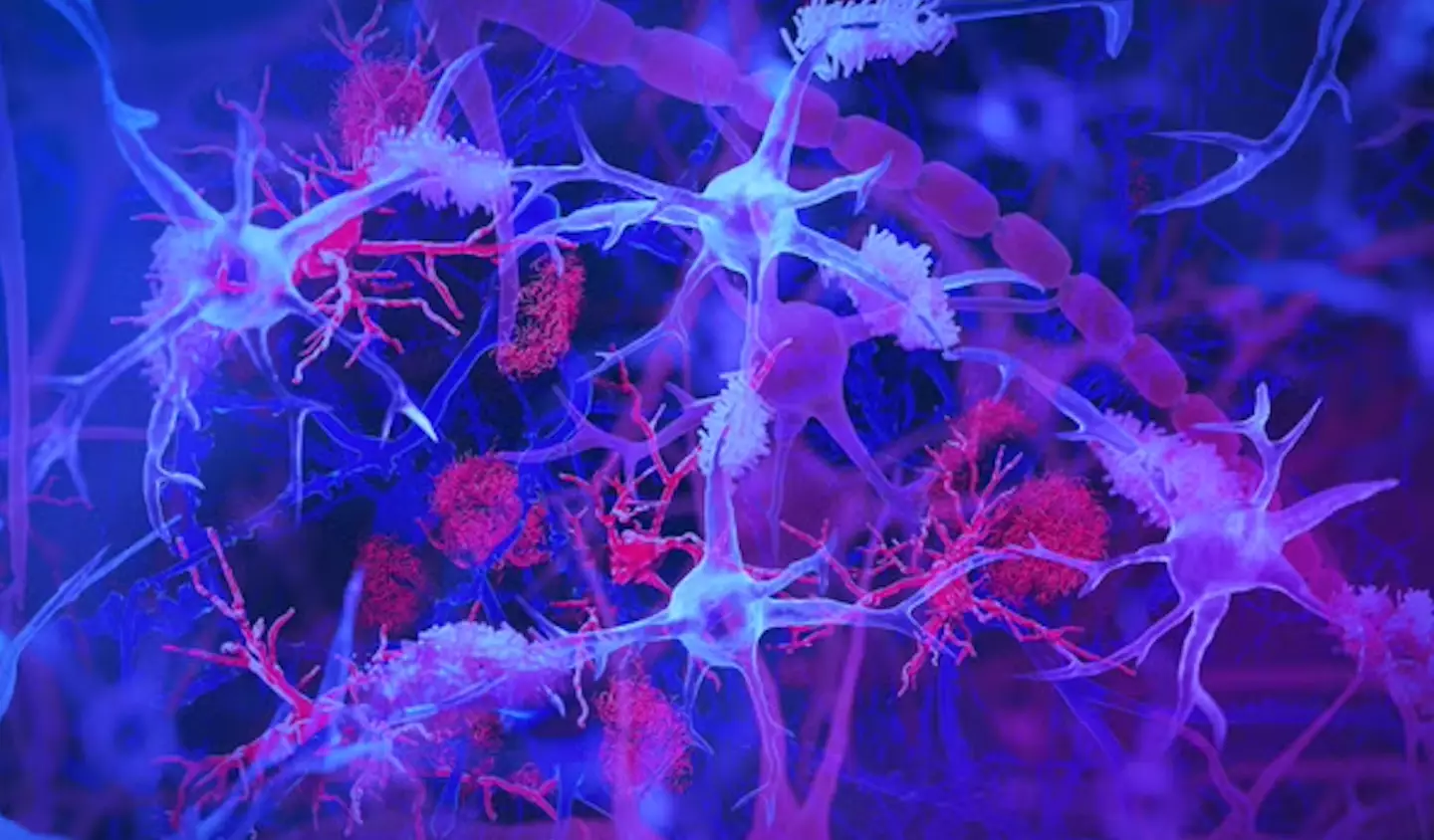
Upon reaching the brain, the virus may alter the immune system and facilitate changes linked with Alzheimer’s disease.
Within the brain, the virus is believed to activate immune cells called microglia to express a gene called CD83, which has been associated with Alzheimer’s in other studies.
Dr. Ben Readhead, co-founder of the study, elaborated on the findings and their potential implications.

He stated: “We think we found a biologically unique subtype of Alzheimer’s that may affect 25-45 per cent of people with this disease.”
Further research is necessary to confirm these findings. Nonetheless, this could lead to new preventive measures against the disease.
Existing antiviral medications might be explored to treat or prevent this specific form of Alzheimer’s disease.
Blood tests currently being developed could potentially identify patients with an active HCMV infection.
Dr. Readhead also noted: “This subtype of Alzheimer’s includes the hallmark amyloid plaques and tau tangles — microscopic brain abnormalities used for diagnosis – and features a distinct biological profile of virus, antibodies and immune cells in the brain.”
